
What to do after a celiac disease diagnosis: Two experts share their tips on long term management, shopping gluten-free, and more
If you had a hunch the chronic symptoms you experienced after eating gluten-based foods pointed to celiac disease and testing with us suggest you might be right, you may be wondering where you go now. Because despite the fact that as many as 1 in every 141 Americans may have celiac disease, there’s often confusion around what exactly celiac disease is, how it can best be managed, and what to do after you’re diagnosed by your healthcare provider.
For starters, celiac disease is often misinterpreted as a food-related condition when it’s actually an autoimmune condition. To further explain the definition of celiac disease and provide clarity on how to take action post-diagnosis, we spoke with Dr. Brett Mendel, MD, of Atlanta Gastroenterology Associates.
“Celiac disease is an autoimmune process where the body reacts to portions of the gluten protein with an immune response,” said Dr. Mendel. “This immune response leads to inflammation that can be seen during endoscopic evaluation and upon microscopic examination of tissue samples. Inflammation also leads to the symptoms experienced by patients with celiac disease. This differentiates celiac disease from food sensitivities where no underlying inflammatory reaction takes place.”
After a celiac diagnosis, you’ll want to switch your diet to gluten-free as early as possible. Once gluten is removed from the diet, Dr. Mendel says approximately 70% of patients will begin to feel better. During this time, the immune response responsible for the inflammation resolves and allows the intestine to heal.
As for the timeline of how long this healing process takes? “Adequate absorption of nutrients can vary from individual to individual, but generally I will test patients for nutrient status 4-6 weeks after they begin a gluten free diet,” said Dr. Mendel.
He also stresses the importance of establishing care with a gastroenterologist and registered dietician for further care and monitoring. This follow-up care can include measures such as baseline upper endoscopy — where a camera is used to evaluate and sample the upper GI tract — or further lab work to monitor nutritional status and response to a gluten-free diet.
According to Dr. Mendel, the addition of vitamins and supplements can be another important piece of post-diagnosis care. “I recommend a good multivitamin, iron supplementation, vitamin D, and B12 supplements be taken for my patients with celiac disease,” he said. “Vitamin levels will need to be followed every 6 months to a year.”
Because the only treatment for celiac disease is to follow a gluten-free diet for life, nutrition plays a crucial role in the long-term management of the autoimmune condition. While navigating that shift isn’t always easy, Registered Dietitian at Rocky Mountain Gastroenterology, Nicole Lindel, says working with a professional or finding a support network can be helpful first steps.
“When I meet with a newly diagnosed celiac disease patient, I start out by acknowledging and validating their feelings, as patients are often very overwhelmed,” said Lindel. “However, there are many resources, support groups, and healthcare professionals, such as registered dietitian nutritionists, that can lighten the load and help guide you through such a drastic change to not only your diet, but also your life.”
As for shopping and navigating foods, Lindel says that thanks to the way the food industry has jumped on the bandwagon of some consumers eating gluten-free diets for “trendiness” rather than necessary health reasons, those with celiac disease can now find gluten free products much easier.
So what should exactly you look for when browsing the shopping aisles — and what should you avoid?
“If a product claims to be ‘gluten free’ on the package, it is most likely safe to eat,” said Lindel. “The FDA allows packaged foods with less than 20 parts per million (ppm) of gluten, including ingredients, cross-contact, and packaging, to be labeled as ‘gluten free.’”
However, there is a catch when it comes to the inclusion of “natural flavors” due to a lack of clarity of what that can include. “If “gluten free” is not indicated on the packaging, you can call the company or err on the safe side and just avoid that particular food item,” she said.
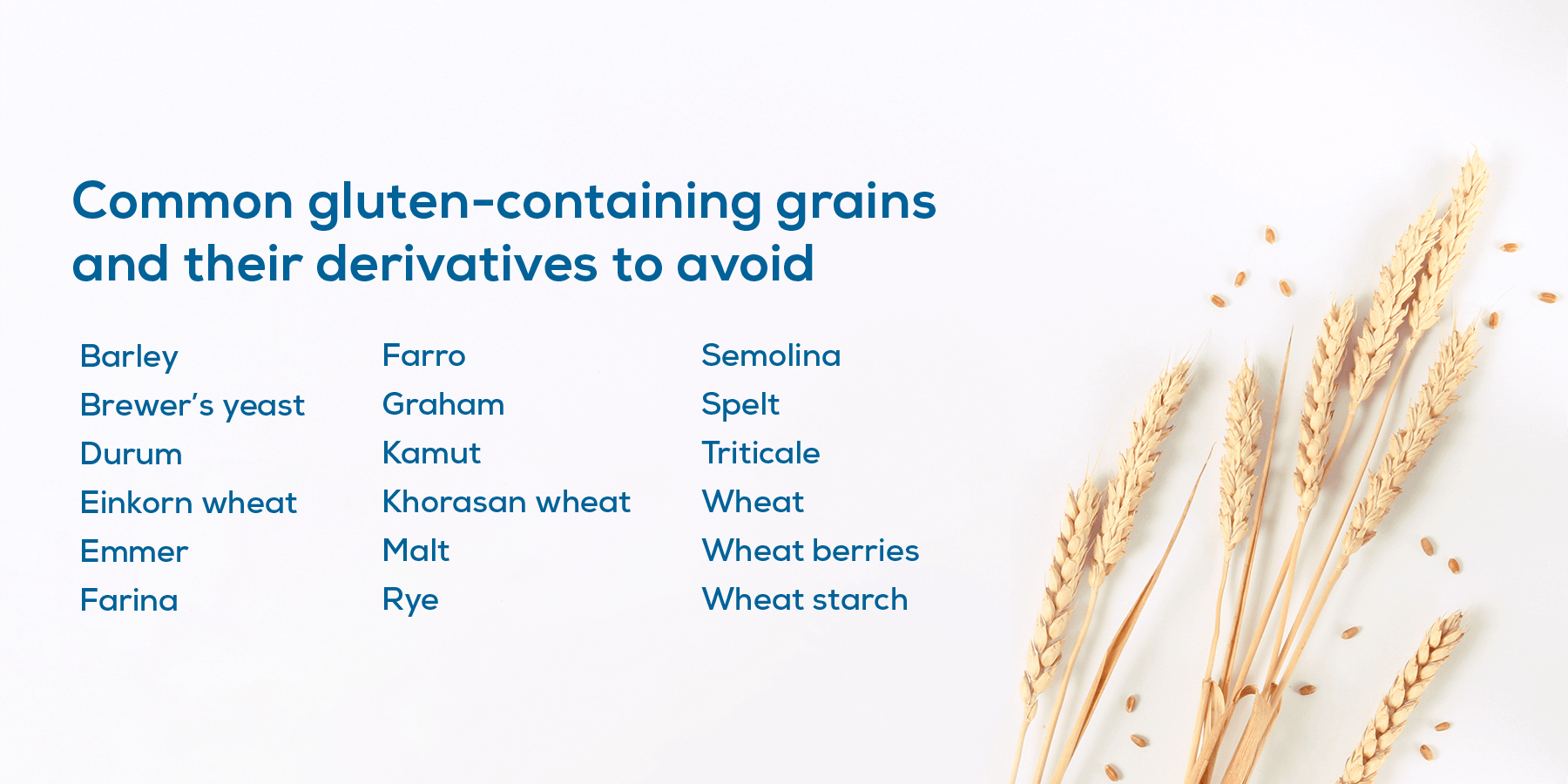

Lindel said that in instances where a product may not list any gluten-containing ingredients but doesn’t clearly use the gluten-free label, there’s still a risk of cross contamination. “If cross contamination is suspected in a patient’s diet, whether it be due to symptoms (bloating, diarrhea, brain fog, fatigue, unintentional weight loss), celiac serologies, or biopsies, sticking exclusively to products labeled as ‘gluten free’ or ‘certified gluten free’ would be advised,” said Lindel.
For those instances where you’re not in control of how food is being prepared, such as when eating at a restaurant or having dinner at a friend’s, Nicole shared some advice on how to best avoid cross-contamination and make eating gluten-free easier.
Here are some tips to follow when eating out and following a gluten free diet:
- Plan ahead! This could include precautions such as calling the restaurant ahead of time, taking a look at their menu, and seeing if they have their own separate gluten free menu.
- When you arrive, share that you have celiac disease. It’s important to note to waitstaff that you follow a gluten free diet due to celiac disease, so measures can be made to prevent cross contamination. Kindly ask your server about gluten free options and if/what measures they take in preparing foods in the kitchen.
- Eating at a friend’s house? Take a backup option. Even with the best intentions, sometimes people don’t understand the risk of cross contamination. By taking something you know is gluten free, you can avoid the risk.
At Everlywell, we’re here to provide you with the support you need post celiac disease diagnosis. If you take our Celiac Disease Screening Test and your results show an indeterminate or increased risk of celiac disease, a member of our patient care department will reach out to you.
In addition to providing you with shareable results, we are here with answers to commonly asked questions about celiac disease and to help prepare you for productive and thoughtful conversations with your healthcare provider.
Resources:
Vici G, Belli L, Biondi M, Polzonetti V. Gluten free diet and nutrient deficiencies: A review. Clin Nutr. 2016 Dec;35(6):1236-1241. doi: 10.1016/j.clnu.2016.05.002. Epub 2016 May 7. PMID: 27211234.