The Use Of At-Home Lab Testing For Preventative Care Access And Stars Improvements
Updated December 8, 2023.
As Medicare Advantage (MA) health plans wrestle with ways to improve Star Ratings during a health crisis that significantly limits in-person care, they find themselves relying heavily on one longstanding initiative: at-home lab tests.
COVID-19’s Impact on In-Person Care
Before COVID-19, in-person interventions were a critical tool in every health plan’s Quality Improvement toolbox, whether sending nurse practitioners to members’ homes to close gaps in care or facilitating in-office appointments between the members and their personal doctors. However, shortly after COVID-19 gained a foothold in the U.S., in-home visits came to a crashing halt and, in many states, physicians began limiting appointments to only those with the most pressing healthcare needs.
In addition to the lack of availability, many MA members simply are not comfortable with in-person interaction. MA members are some of the more at-risk members of society when it comes to COVID-19. As a result, these members understandably have a high amount of anxiety regarding in-person interactions of any kind, including healthcare. The likelihood of foregoing preventive care – and even chronic care – is high. In fact, a recent report by Epic Health Research Network, found that screening appointments were down 86%-94% in March, compared to usual volumes [1].
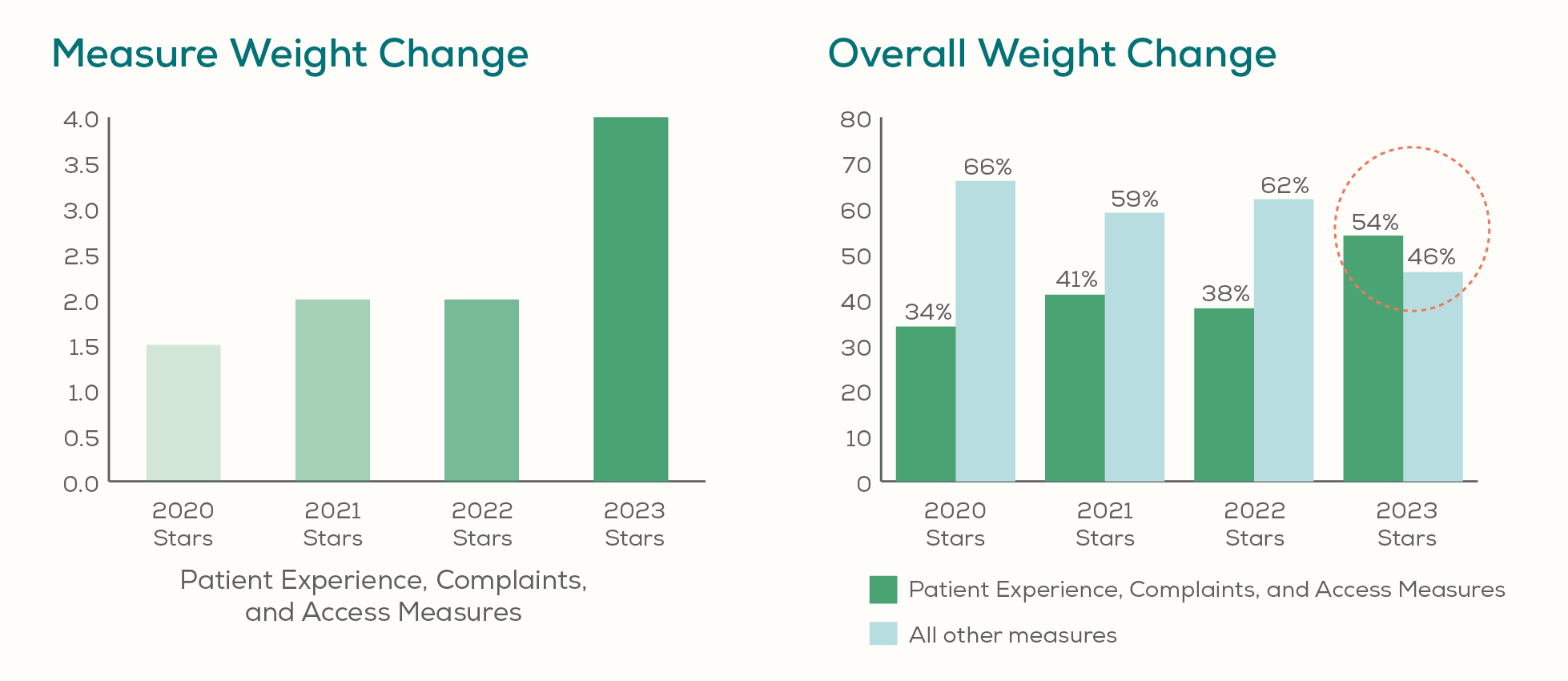
To counter these trends and to ensure access to care for their members, MA plans turned to virtual and non-invasive care. The explosive adoption of virtual care has been well documented, but the lift provided through at-home lab tests has also been significant. And though it’s too early to see the impact on the actual measures from the Medicare Consumer Assessment of Healthcare Providers and Systems (CAHPS®) survey, plans who have proactively made virtual and non-invasive care more accessible to their members are likely creating more satisfied members, as well as building more trust with them. This is important as the Medicare Stars patient experience, complaint, and access measures are increasing to a weight of 4 starting with 2021 calendar year performance.
By comparison, intermediate clinical outcome measures, such as the percentage of a plan’s diabetic members effectively managing their blood sugar, are only a weight of 3.
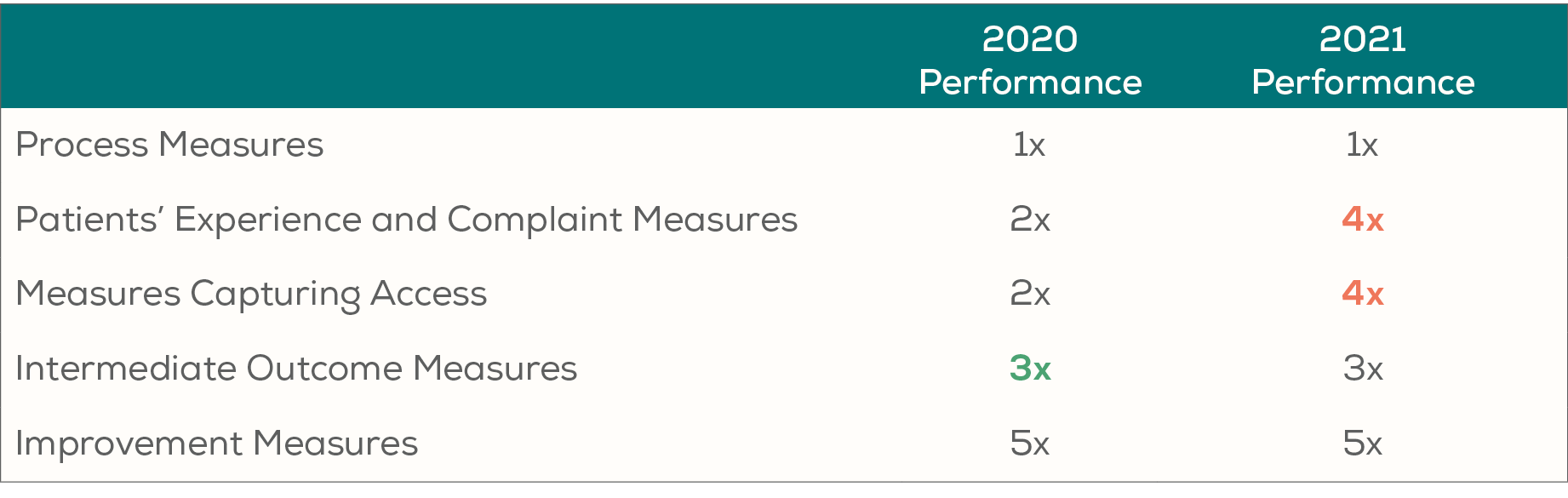
With this change, these experience measures will comprise more than half of a health plan’s Star Rating for the first time.
Health plans understand that Star Ratings are graded on a curve. Plans must perform better than their peers across the industry across most of these measures to receive high Star Ratings and the significant revenue that comes with them.
Ability of At-Home Lab Tests to Close Gaps in Care
For three specific measures from the Healthcare Effectiveness Data and Information Set (HEDIS), at-home lab tests effectively close the gap in care and help the plan increase its compliance rate.
Colorectal Cancer Screening
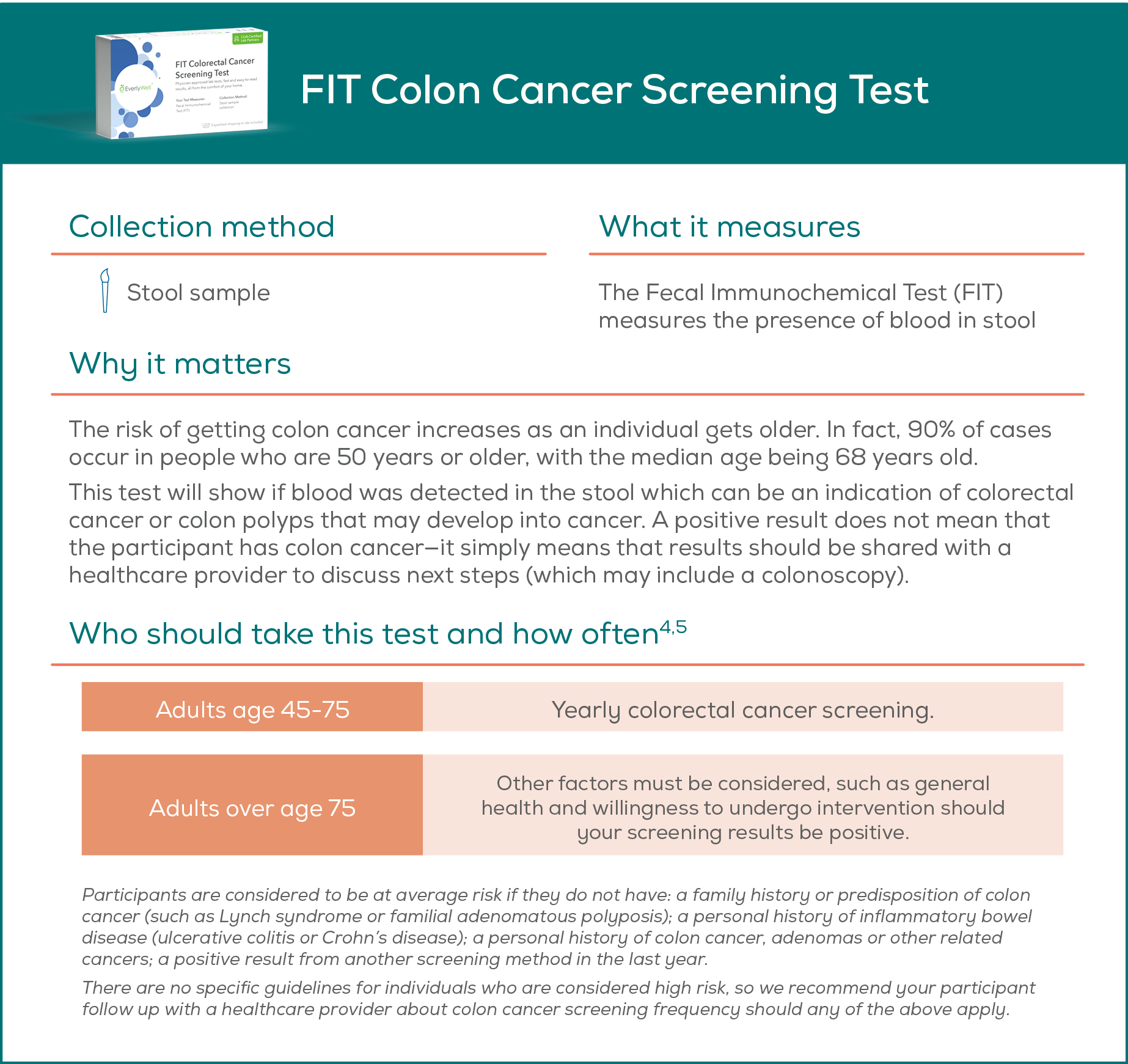
According to the IQVIA Institute in an April 2020 study, three months of missed or delayed testing resulting from COVID-19’s disruption to healthcare could lead to over 80,000 positive cancer diagnoses [2].
Colorectal Cancer Screening is a HEDIS measure with a weight of 1. It assesses adults 50–75 who had appropriate screening for colorectal cancer with any of the following tests: annual fecal occult blood test, flexible sigmoidoscopy every 5 years, colonoscopy every 10 years, computed tomography colonography every 5 years, stool DNA test every 3 years [3].
Two of these appropriate screenings are an annual Fecal Occult Blood Test (FOBT) or Fecal Immunochemical Test (FIT), which can be conducted in the member’s home with no in-person human interaction.
The at-home colon test (fecal immunochemical test) typically consists of a stool sample collection that is mailed back to a lab for processing.
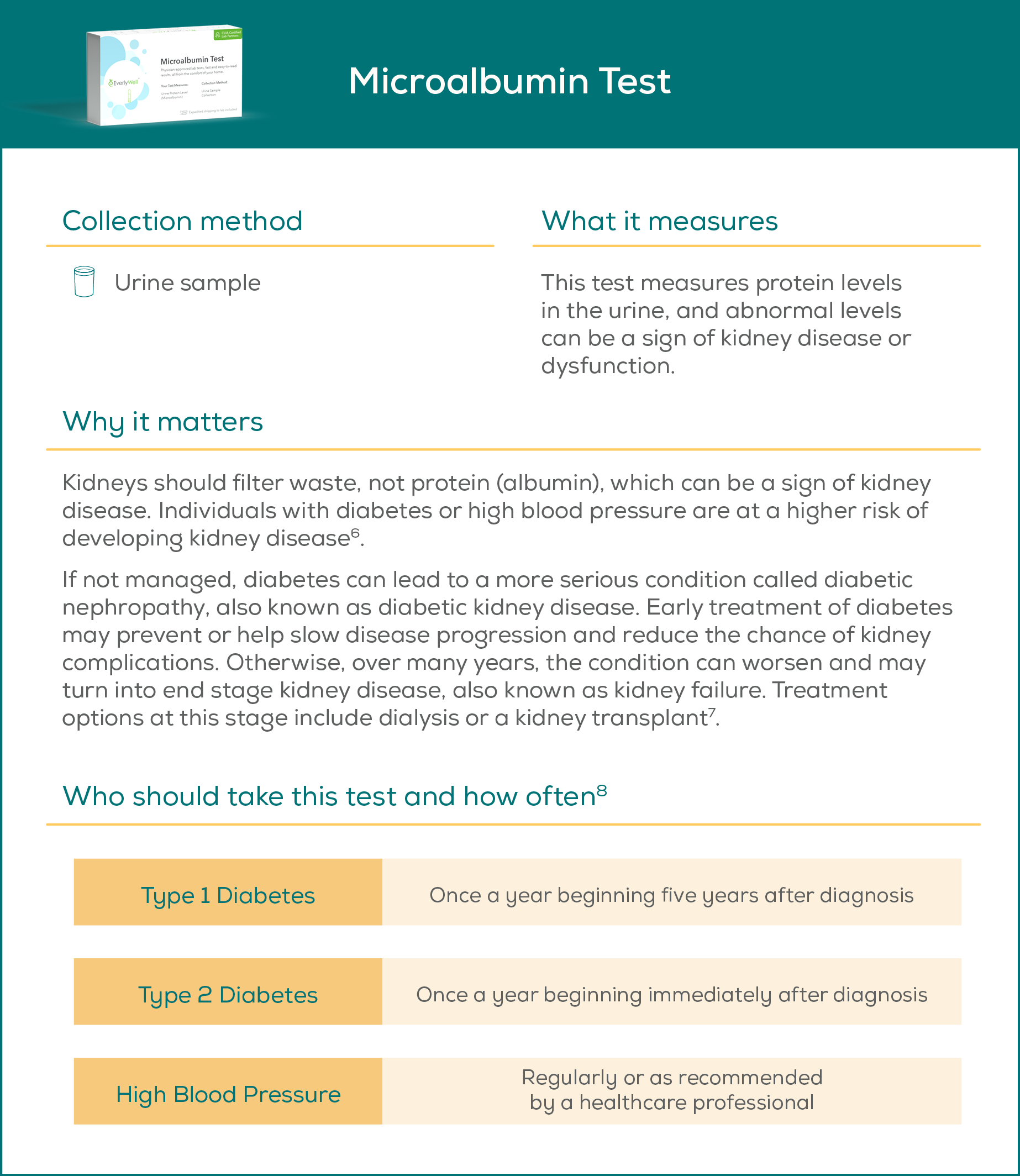
Diabetes Care – Kidney Disease Monitoring
This is a HEDIS measure with a weight of 1 focused on kidney function testing for members with diabetes. It measures adults 18-75 years of age with type 1 or type 2 diabetes who have had medical attention for nephropathy during the measurement year, this includes assessments of kidney function and kidney damage. An at-home microalbumin test can be used to fulfill the assessment of kidney damage requirement.
The at-home lab test typically consists of a urine sample collection that is mailed back to a lab for processing.
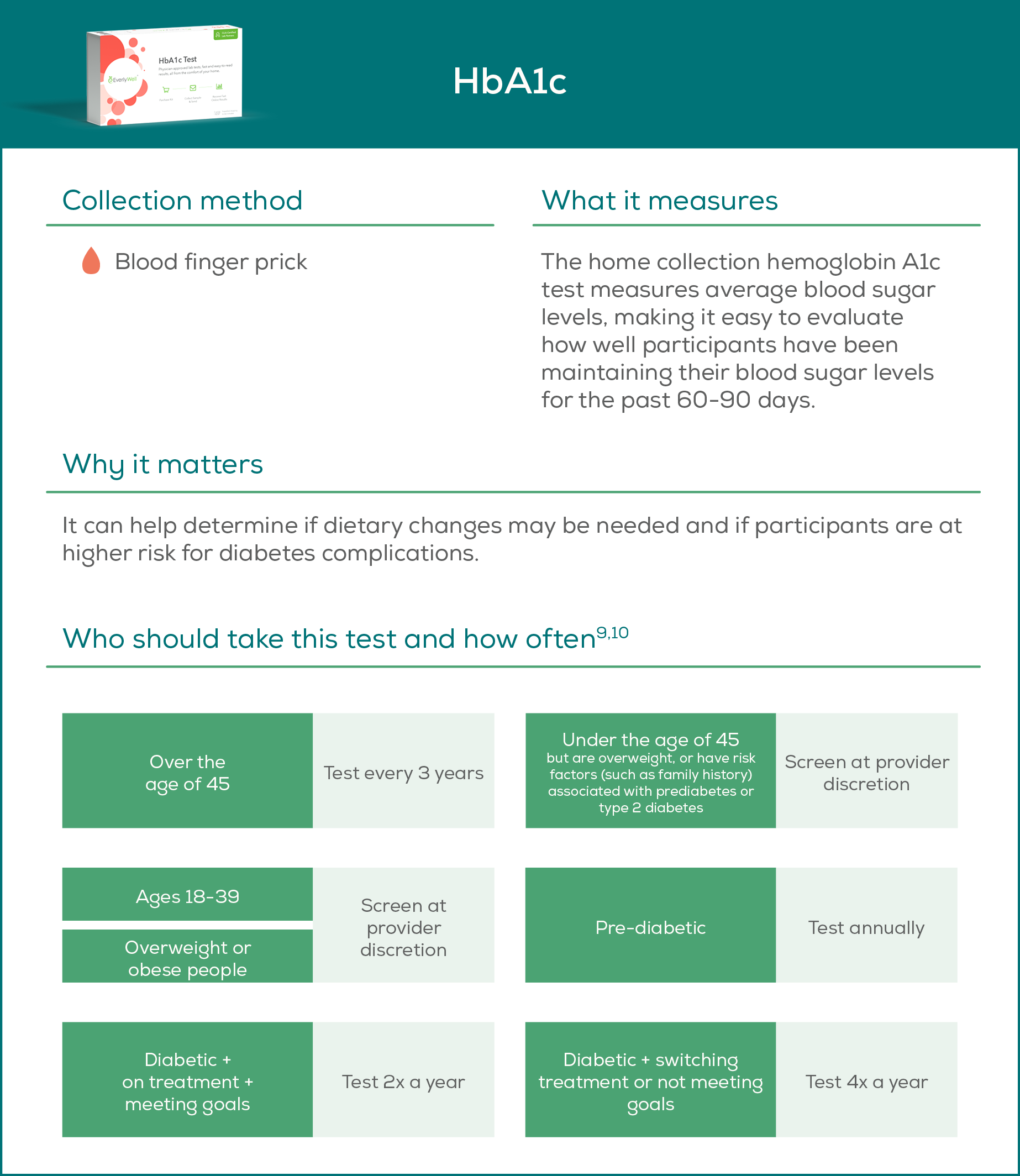
Diabetes Care – Blood Sugar Controlled
This is a HEDIS measure with a weight of 3 focused on plan members with diabetes whose blood glucose is under control. It measures the percentage of diabetic MA enrollees 18-75 years of age who had a HbA1c test during the measurement year and demonstrate good control (<=9%).
The at-home lab test typically consists of a finger prick blood test that is mailed back to a lab for processing.
Potential Member Experience Impact of At-Home Lab Tests
Not only do at-home lab tests provide an effective way to close gaps in care, they potentially provide a way to do so in a manner that results in a positive member experience that can influence the patient experience measures.
At-home lab tests inherently provide certain appealing benefits to health plan members. For example, they are convenient and help to overcome transportation barriers that might exist.
In a COVID-19 world, the fact that the tests can be conducted in a non-invasive manner with no in-person interaction and no one having to come to the member’s home (and no potential exposure) can significantly reduce member anxiety and help ensure they are obtaining important care, whether it be preventive or management of chronic conditions.
However, regardless of how convenient and non-invasive these tests might be, they still have the potential to create a very negative experience if certain key facets of the experience are lacking. To provide a positive experience, the at-home test experience needs to include flawless execution of the steps below.
Members who need the test receive outreach that accomplishes the following:
- Educates them on the importance, convenience, and credibility of the test
- Invites them to receive the test, collect their sample from the safety of their home, mail it back for processing at the lab, and then receive informative results and insights
- If applicable, informs the member of the reward or incentive they will receive from their health plan for completing the test
The test should arrive when the member expects it to arrive
Simple sample collection experience
-
Directions accompanying the test are easy to understand regarding how to complete it and return it
-
Should the member have any questions, they should be able to contact a support team and receive quick, accurate, and courteous assistance
-
Results of the test are provided timely to the member via digital platform and/or mail, based on the member’s preference
-
Results are informative, effectively communicate the meaning of the test results, and include helpful recommendations to take action towards better health
-
Participant results are also provided to the member’s personal doctor and to the health plan
Providing the results to the member’s personal doctor, and not requiring the member to do so, is important for coordination of care to take place. Care Coordination is an actual Star Ratings measure that can potentially be positively influenced by making the personal doctor aware of all care and tests that the member receives.
Care Coordination
Care Coordination is a CAHPS survey measure with a weight of 2 currently. As a patient experience measure, it is increasing to a weight of 4 for 2021 calendar year performance. The score for the measure is a composite based on six questions from the CAHPS survey. As shown below, these questions ask if the members received their test results, if they received them when they needed them, and if their personal doctor was informed about other care they had received.
- In the last 6 months, when you visited your personal doctor for a scheduled appointment, how often did he or she have your medical records or other information about your care?
- In the last 6 months, when your personal doctor ordered a blood test, x-ray or other test for you, how often did someone from your personal doctor’s office follow up to give you those results?
- In the last 6 months, when your personal doctor ordered a blood test, x-ray or other test for you, how often did you get those results as soon as you needed them?
- In the last 6 months, how often did you and your personal doctor talk about all the prescription medicines you were taking?
- In the last 6 months, did you get the help you needed from your personal doctor’s office to manage your care among these different providers and services?
- In the last 6 months, how often did your personal doctor seem informed and up-to-date about the care you got from specialists?
Leveraging At-Home Lab Tests
If executed effectively, at-home lab tests provide an effective way to improve Star Ratings, both from a clinical gap in care perspective and a patient experience perspective. These tests should be an important part of every health plan’s Quality Improvement plan. Now it's even easier (and more affordable) to use at-home lab tests regularly with Everlywell + testing membership. Monitor your HbA1c levels, screen for colon cancer, test for STDs, and more as often as once a month, and for as as little as $39/month. Learn more about Everlywell+.
About the Author
Rex Wallace is the founder and principal of Rex Wallace Consulting, LLC (RWC), a firm that specializes in improving Star Ratings for Medicare Advantage health plans.
Rex assesses plans and guides them in the development and implementation of industry-leading strategies to drive material Quality Improvement. Since its inception in 2017, RWC has helped multiple Medicare Advantage contracts achieve significant improvements in Star Ratings, including single-year full-Star improvements.
Prior to launching RWC, Rex spent twenty-three years in strategic healthcare roles, with a strong focus on Medicare Advantage. Most recently, he led Stars for a large, multi-state plan that consistently achieved 4 and 4.5 Stars across its multiple contracts.
References
1. Epic Health Research Network . Preventive cancer screenings during COVID‐19 pandemic. Published 2020. URL.
2. Murray A and Kleinrock M. Shifts in healthcare demand, delivery and care during the COVID-19 era. IQVIA Institute for Human Data Science. April 2020.
3. American Cancer Society. 2017. “Colorectal Cancer Facts & Figures 2017-2019.” URL.
4,5. Centers for Disease Control and Prevention. Colorectal Cancer Screening Tests. URL.
6, 7. Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2019
8. Microalbumin test. URL (2018, December 19).
9,10. Centers for Disease Control and Prevention. All About Your A1C. URL (2018, August 21).
Originally published December 14, 2020.