How Many Types of HPV Are There?
Medically reviewed on January 10, 2022. To give you technically accurate, evidence-based information, content published on the Everlywell blog is reviewed by credentialed professionals with expertise in medical and bioscience fields.
Human papillomavirus infection, or HPV, is the most common sexually transmitted infection. Estimates suggest that around 79 million people in the United States currently have HPV and that 80 percent of sexually active people will become infected at some point in life [1].
These statistics can sound alarming, but HPV is usually harmless. HPV symptoms can also look different in each person, and some can have HPV without symptoms. Most people with HPV show no symptoms and feel fine, and the infection typically goes away on its own. However, there are hundreds of different strains of HPV, and some of these strains are more harmful than others. Read on to learn more about HPV and its different types below (and consider learning more about the at-home HPV Test).
What is HPV?
While HPV is the most common STI, not all forms of HPV are spread via sexual contact. Oftentimes, skin-to-skin contact is enough to spread the virus. Certain types of HPV only affect the hands, leading to hand warts or cause plantar warts on the feet. About 40 types of HPV can infect the genitals, including the vagina, vulva, cervix, penis, scrotum, rectum, or anus. These strains can also potentially infect the mouth, lips, or throat [2].
As mentioned, HPV most commonly spreads through sexual contact, meaning that you can get it when the genitals contact someone else’s genitals or mouth. The virus can still spread even if no one orgasms [2].
Symptoms of HPV
For most people, HPV will present no meaningful or even apparent symptoms. You may have the virus and feel perfectly fine, though this is partly why the virus can spread so easily. However, the bigger concern is that even high-risk forms of HPV don’t present with any noticeable symptoms until it has already proceeded to more severe stages. High-risk forms of HPV increase the risk of cancer [3]. HPV is most commonly linked to cervical cancer, but a high-risk HPV infection can also increase the risk of other forms of HPV related cancer, including:
- Vulvar cancer
- Anal cancer
- Penile cancer
- Throat cancer
High-risk HPV doesn’t always turn into cancer, and it can take several years for cancer to develop. With an HPV test, you can isolate and identify the HPV before it becomes an issue [3].
Outside of an increased risk of cancer, some people who contract HPV may develop warts. These growths can appear anywhere on the infected area, including the hands, feet, and genitals. Some low-risk forms of HPV may also cause mild cervical dysplasia. This refers to abnormal growths on the surface of the cervical wall, but these growths are not considered precancerous [4].
Types of HPV
There are hundreds of HPV strains, which are identified by a number. These strains are usually split into high-risk (meaning they can potentially lead to cancer) and low-risk [4]. Most estimates suggest that there are more than 200 known types of human papillomavirus, and about 40 of those strains can infect the genital area, mouth, and throat. Two types of HPV, types 6 and 11, are the most common cause of genital warts [2].
About a dozen different types of HPV can potentially result in cancer. HPV types 16 and 18 are the strains that most commonly lead to cancer [2].
Again, most types of HPV do not pose any serious health risks. However, it is possible for a person to contract more than one type of HPV at a time [4].
Testing for HPV
Because HPV is so common, regular testing may be a good option if you are sexually active. While there aren’t any tests for other genital areas, you can get an HPV test for the cervix, which can help identify and prevent cervical cancer [5].
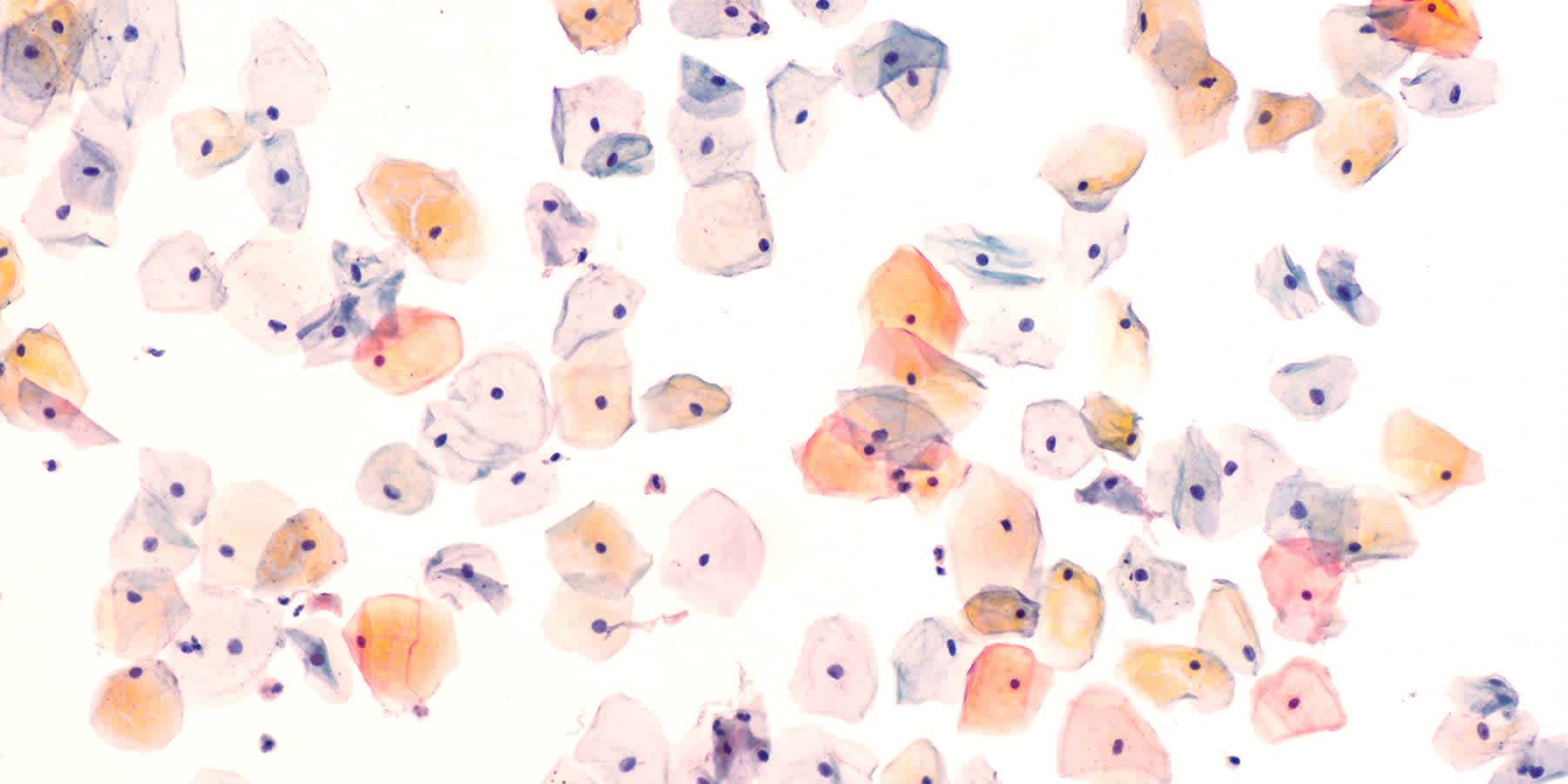
HPV tests can be a regular part of a wellness exam. During the test, a nurse or gynecologist places a speculum into the vagina. The speculum separates the walls of the vagina, which allows the gynecologist to take a small sample of cells from the cervix using a brush or tiny spatula. This process takes just a few minutes, and while there may be discomfort, it shouldn’t be painful. Once the gynecologist or nurse has collected the cells, the sample is sent to a lab for testing. HPV tests specifically look for high-risk types of HPV, including types 16 and 18 [6].
Alternatively, or in conjunction with the HPV test, you may get a Pap test, also known as a Pap smear. A Pap smear tests for small changes in the cervical cells that may point to abnormalities associated with cancer. However, Pap tests do not specifically detect HPV. The sample collection process for a Pap smear is the same as an HPV test and can be performed consecutively [7].
The frequency of these tests can vary from person to person. Generally, most gynecologists recommend getting an HPV test every five years for women ages 25 to 65. In areas where HPV tests are not available, your gynecologist may recommend a Pap test every three years for the same age group [7].
If an HPV or Pap test comes back with abnormal results, a gynecologist can perform a colposcopy. This test looks even closer at cervical cells to determine if they show any abnormalities and, if so, the extent. If they notice something abnormal, they can take a biopsy, or a small sample of tissue, which is sent to a lab for further testing [8].
Treatments for HPV
There is currently no known cure for an HPV infection. Most HPV infections go away on their own, though, and the body’s immune system can typically fight off infections before they present any noticeable symptoms [9].
If you develop warts of any kind, your healthcare provider can typically remove them via surgery, including cryotherapy (freezing the warts off) or electrocautery (burning them with an electrical current) [10].
More commonly, a healthcare provider will prescribe topical medication. Applied directly to the wart, topical medication can gradually remove the lesion over time. Common topical treatments include salicylic acid, podofilox, and imiquimod [10].
If the results of a Pap test, HPV test, or colposcopy come back abnormal, the healthcare provider can potentially remove precancerous cells before they become fully cancerous. This may involve cryotherapy or loop electrosurgical excision procedure (LEEP) [9].
Preventing Types of HPV
One of the best things you can do to prevent HPV is to get an HPV vaccine. Everyone from the age of 9 to 45 can receive the HPV vaccine. The HPV vaccine, also known as Gardasil 9, can protect against the types of HPV that most commonly increase the risk of cancer and genital warts, including:
- Types 6 and 11
- Types 16 and 18
- Types 31, 33, 45, 52, and 58
The vaccine is administered via a series of shots. For those aged 9 to 14, this involves just two shots, with the second dose given six months after the first dose. For those aged 15 and older, three shots are required. The second shot is given two months after the first dose, and the third dose is given four months after the second dose [11].
While an HPV vaccination can be beneficial, practicing safer sex can also help to reduce your risk of HPV. This includes using dental dams and condoms any time you have oral, anal, or vaginal sex.
The biggest problem with any HPV type is that most people never know that they’re infected in the first place. While that’s fine for most forms of HPV, it’s still a good idea to get tested to prevent spreading the virus to your sexual partners. The Everlywell HPV Test offers women an at-home test that screens for 14 high-risk forms of HPV, including types 16 and 18, to help keep you and your partner(s) safe and healthy.
Related content
What are the symptoms of HPV in females?
What are the symptoms of HPV in males?
References
1. HPV (Human Papilloma Virus). Cleveland Clinic. URL. Accessed January 10, 2022.
2. Human Papillomavirus (HPV). Planned Parenthood. URL. Accessed January 10, 2022.
3. What are the symptoms of HPV? Planned Parenthood. URL. Accessed January 10, 2022.
4. Types of Human Papillomavirus. NYU Langone. URL. Accessed January 10, 2022.
5. Should I get tested for HPV? Planned Parenthood. URL. Accessed January 10, 2022.
6. What's an HPV test? Planned Parenthood. URL. Accessed January 10, 2022.
7. What's a Pap test? Planned Parenthood. URL. Accessed January 10, 2022.
8. What is a colposcopy? Planned Parenthood. URL. Accessed January 10, 2022.
9. How is HPV treated? Planned Parenthood. URL. Accessed January 10, 2022.
10. HPV infection: diagnosis, treatment. Mayo Clinic. URL. Accessed January 10, 2022.
11. Should I get the HPV vaccine? Planned Parenthood. URL. Accessed January 10, 2022.