Tick Bites: How To Treat, Recognize Symptoms, and Prevent
Medically reviewed on June 7, 2022 by Jordan Stachel, M.S., RDN, CPT. To give you technically accurate, evidence-based information, content published on the Everlywell blog is reviewed by credentialed professionals with expertise in medical and bioscience fields.
While the spring, summer, and fall months are optimal for enjoying the outdoors, they also have the best conditions for ticks. If you’ve spent time in wooded or grassy areas while hiking or camping, you may have encountered ticks before—and been at risk for tick bites.
Although most ticks are harmless, some tick bites can transmit bacteria that cause illnesses like Lyme disease and Rocky Mountain spotted fever in both humans and pets. With camping season in full swing, we’ve outlined everything you need to know about how to treat a tick bite and what to do after finding one on yourself or your pet.
Read on or skip to our camping printables to ensure both you and your pets stay safe and healthy in the outdoors.
Table of Contents
- How To Safely Remove a Tick
- How To Treat Tick Bites
- Lyme Disease vs. Rocky Mountain Spotted Fever
- When To Call a Healthcare Provider
- How To Prevent Tick Bites and Infections
- Tick Prevention for Pets
- How To Protect Kids From Ticks
How To Safely Remove a Tick
It can be tempting to simply pull a tick off immediately after spotting it, but it’s important to take the proper precautions to prevent injury and ensure that you don’t leave parts of the tick behind. If you notice a tick has latched onto you or your pet’s skin, follow these steps to safely remove it:
1. Use Fine-tipped Tweezers
It’s important to make sure you get your removal tool as close to the skin as possible so that you can pull off the body of the entire tick. Leaving parts of the tick’s body in your skin can cause infection. For pets, spread their fur apart before grasping the tick to ensure you are close to the skin.
2. Gently Pull the Tick Upward
Avoid using remedies such as painting the tick with nail polish, using petroleum jelly, or applying heat to get the tick to detach itself. These methods take much longer, and using heat could injure your skin. You’ll want to remove the tick as soon as possible and not wait for it to detach, as giving the tick more time to salivate on your skin may increase your risk of contracting an illness.
3. Seal the Tick in a Bag or Container
If you would like to bring the tick to your healthcare provider for testing, place it in rubbing alcohol to make sure it’s killed, then seal it in a bag or container.
How To Treat Tick Bites
Treating a tick bite as soon as possible can help prevent infection and reduce your risk of contracting Lyme disease or Rocky Mountain spotted fever. To treat a tick bite, follow these steps:
1. Clean the Affected Area
Once you have disposed of the tick, it’s important to thoroughly wash your hands and clean the bite area with soap and water. You can also gently clean the area with rubbing alcohol to reduce the risk of infection.
2. Check for Pieces Still Attached to the Skin
In some cases, ticks can burrow into the skin and leave behind parts of their head or mouth when you try to remove them. If you see pieces still attached to your skin after pulling off the tick, try to gently remove them using fine-tipped tweezers or a tick removal tool. Leaving small pieces behind could further irritate the skin and increase your risk of infection.
3. Use an Ice Pack
Tick bites are generally painless but can cause slight swelling or tenderness in some people. If the bite area is sore, you can apply a cold compress for 10 to 15 minutes every hour or two. Just remember to put a thin cloth between the ice and your skin to prevent further irritation.
4. Try Over-the-Counter Antihistamines
Tick bites can sometimes cause itching and swelling. To relieve itching, you can use an over-the-counter medication like Benadryl or a topical itch relief ointment. However, you should ask your healthcare provider first if you have never used them before or are prone to allergic reactions. Be sure to carefully read the instructions on the label and stop using the product immediately if you have a reaction.
Symptoms of Lyme Disease vs. Rocky Mountain Spotted Fever

After experiencing a tick bite, healthcare providers recommend observing yourself for symptoms for up to 30 days. Distinctive rashes are the first signs of infection for both Lyme disease and Rocky Mountain spotted fever (RMSF). For Lyme disease, a rash may appear within 3 to 30 days of a tick bite and typically before the onset of a fever. For RMSF, a rash may develop within 2 to 5 days of a tick bite and after the onset of a fever.
Important note: If you develop a circular rash or a spotted rashe, you should see your healthcare provider immediately as it could be a sign of Lyme disease or Rocky Mountain spotted fever.
Lyme Disease Symptoms
Lyme disease is the most common vector-borne disease in teh United States. It’s caused by a bacteria called Borrelia burgdorferi, and sometimes Borrelia mayonii, which are both transmitted by blacklegged ticks. Most cases of Lyme disease are treated with antibiotics, and experts agree that the sooner you’re treated, the better. Conversely, untreated Lyme disease can spread to other parts of your body, causing arthritis and nervous system problems.
Anyone who has been bitten by a tick is at risk of contracting Lyme disease. That said, it’s important to monitor yourself for symptoms to determine if a Lyme disease test or treatment is needed.
Common Lyme disease symptoms in humans: circular, expanding rash with a bull’s-eye pattern Erythema migrans (EM) rash, fever, chills, headache, fatigue, muscle and joint aches, neck stiffness, facial palsy, heart palpitations or irregular heartbeat Lyme carditis, episodes of dizziness or shortness of breath, nerve pain, inflammation of the brain and spinal cord, and shooting pains, numbness, or tingling in the hands or feet
Common Lyme disease symptoms in pets]: fever, loss of appetite, reduced energy, lameness (can be shifting, intermittent, or recurring), generalized stiffness, and joint swelling and discomfort
Rocky Mountain Spotted Fever Symptoms
Rocky Mountain spotted fever is another harmful bacterial disease spread through ticks. Unlike Lyme disease, RMSF is transmitted through several different species of ticks, including the American dog tick, Rocky Mountain wood tick, and the brown dog tick. This bacterial disease may cause individuals to get a red, spotted rash and high fever upon infection.
While RMSF was first identified in the Rocky Mountains, it’s most commonly found in the southeastern part of the United States. Ticks carrying this disease can also be found in parts of Canada, Mexico, and both Central and South America. Many people affected by RMSF may become sick after the first week of infection. For others, however, signs and symptoms may not appear for up to 14 days.
Common RMSF symptoms in humans: spotted rash, high fever, chills, severe headache, muscle aches, nausea and vomiting, and confusion or other neurological changes
Common RMSF symptoms in pets: poor appetite, muscle or joint pain, fever, coughing, abdominal pain, vomiting, diarrhea, swelling in the face or legs, and depression
When To Call a Healthcare Provider
If you begin experiencing flu-like symptoms, develop a rash, or notice any other signs of Lyme disease or Rocky Mountain spotted fever, you should make an appointment with your healthcare provider right away. These conditions require antibiotics and can cause serious complications if left untreated.
You should also contact a healthcare provider if you suspect that the bite is infected or you aren’t able to completely remove the tick from your skin. Common signs of infection include swelling and inflammation, pain, and oozing from the bite site.
How to Prevent Tick Bites and Infections

While ticks are most common from April to September, they can be present year-round. Tick prevention can go a long way in protecting you, your loved ones, and your pets from being bitten and contracting an illness. If you’re spending time outdoors this year, be sure to follow these five simple tips for preventing tick bites:
1. Avoid Areas Where They Live
Ticks live in grassy, bushy, and wooded areas—and may even live on other animals. When spending time outdoors, do your best to avoid areas that are hot spots for ticks, such as heavily wooded or grassy areas, especially during tick season (April–September).
2. Wear Protective Clothing
Permethrin is an effective pesticide that kills and repels insects like ticks and mosquitos. Wearing permethrin-treated clothing and gear can help reduce your risk of a tick bite. The CDC also recommends treating your own clothes and boots with products containing 0.5% permethrin, and they will remain protective through several washes. If weather permits, wearing clothing that covers your arms and legs can also help prevent tick bites.
When outdoors with pets, make sure they are wearing a tick collar or are up to date on tick prevention medications.
3. Use EPA-registered Insect Repellents
Insect repellents are a quick and easy way to prevent ticks bites. When outdoors, use Environmental Protection Agency (EPA)-registered insect repellents that are verified to be effective and safe for your skin. These products will have an EPA registration number (EPA Reg. No.) on the label. You can use the EPA’s online tool to help you identify which type of repellent is best for you, based on how long you need protection and what insect you need protection from.
Products that have not been registered with the EPA have not been evaluated for effectiveness and may not provide adequate protection against ticks and tick-borne illnesses. Examples of ingredients used in unregistered insect repellents include citronella oil, cedar oil, geranium oil, peppermint/peppermint oil, and soybean oil.
While insect repellents are often the simplest way to deter ticks and other insects from biting you, it’s important to note effectiveness can vary due to the following conditions: physical activity/sweating, exposure to water, and the temperature outside. That said, it’s best not to rely on insect repellent alone to reduce your risk of tick bites.
4. Check Gear, Skin, and Clothing for Ticks
After spending time outside or being in a potentially tick-infested area, you should always check your skin, clothing, and gear for ticks. This way, you may be able to catch a tick before it latches onto you. If you find a tick, safely remove it immediately.
The CDC suggests that you tumble dry your clothes on high heat for 10 minutes to further kill any ticks that may be hidden in your clothing. Make sure you use hot water when washing, as cold and medium temperatures will not kill ticks.
5. Shower After Being Outdoors
When you come inside, be sure to shower and thoroughly wash your body. Showering within two hours of coming indoors has been shown to reduce the risk of contracting Lyme disease and may be effective in reducing the risk of other tick-borne diseases.
Tick Prevention for Pets
Many pets love to spend time outdoors, so you should routinely check them for ticks. Remember, ticks can migrate between hosts, so it’s possible for pets to bring ticks to their owners or other pets.
If you have a pet, be sure to follow these prevention practices to reduce the risk of a bite and/or tick-borne illness for you and your pet:
- Regularly bathe your pet with lukewarm water and tick shampoos that are formulated to kill live ticks upon contact.
- With a fine-toothed comb, brush areas where ticks will burrow on your pet, like around the ears, between the legs, between the toes, under the front legs, and around the tail.
- Reduce tick habitats in your yard by keeping grass trimmed and applying pet-safe pesticides.
- Keep pets up to date on veterinarian-approved flea and tick medications.
How To Protect Kids from Ticks
If you have children, there are a few steps you can take to help protect them from tick bites during outdoor activities:
- Teach them which areas to avoid. Ticks thrive in moist, shady environments and often cling to tall grass and shrubs.
- Dress them in long pants and long sleeves if weather permits to protect their arms and legs from ticks.
- Teach them to check themselves for ticks. Some of the most important areas to check are ankles, knees, underarms, ears, the hairline, and around the waist.
- Apply an EPA-registered insect repellent before spending time outside.
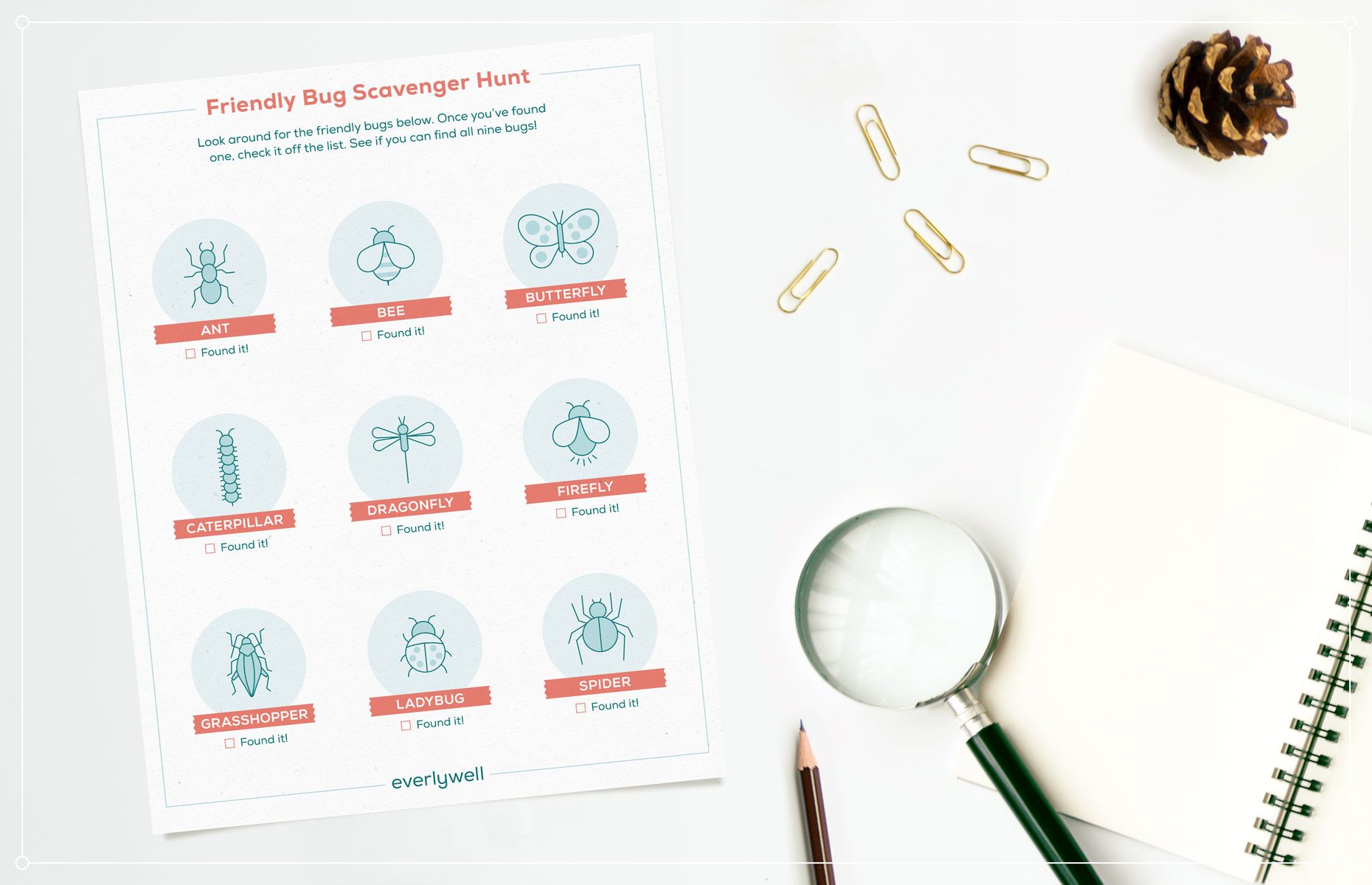
That said, not all bugs are harmful and dangerous—and if you’re being safe, camping should be enjoyable for everyone. If you’re camping with kids this year, we’ve created a fun printable activity for little ones to spot friendly critters and learn which types of bugs should be avoided when outdoors.
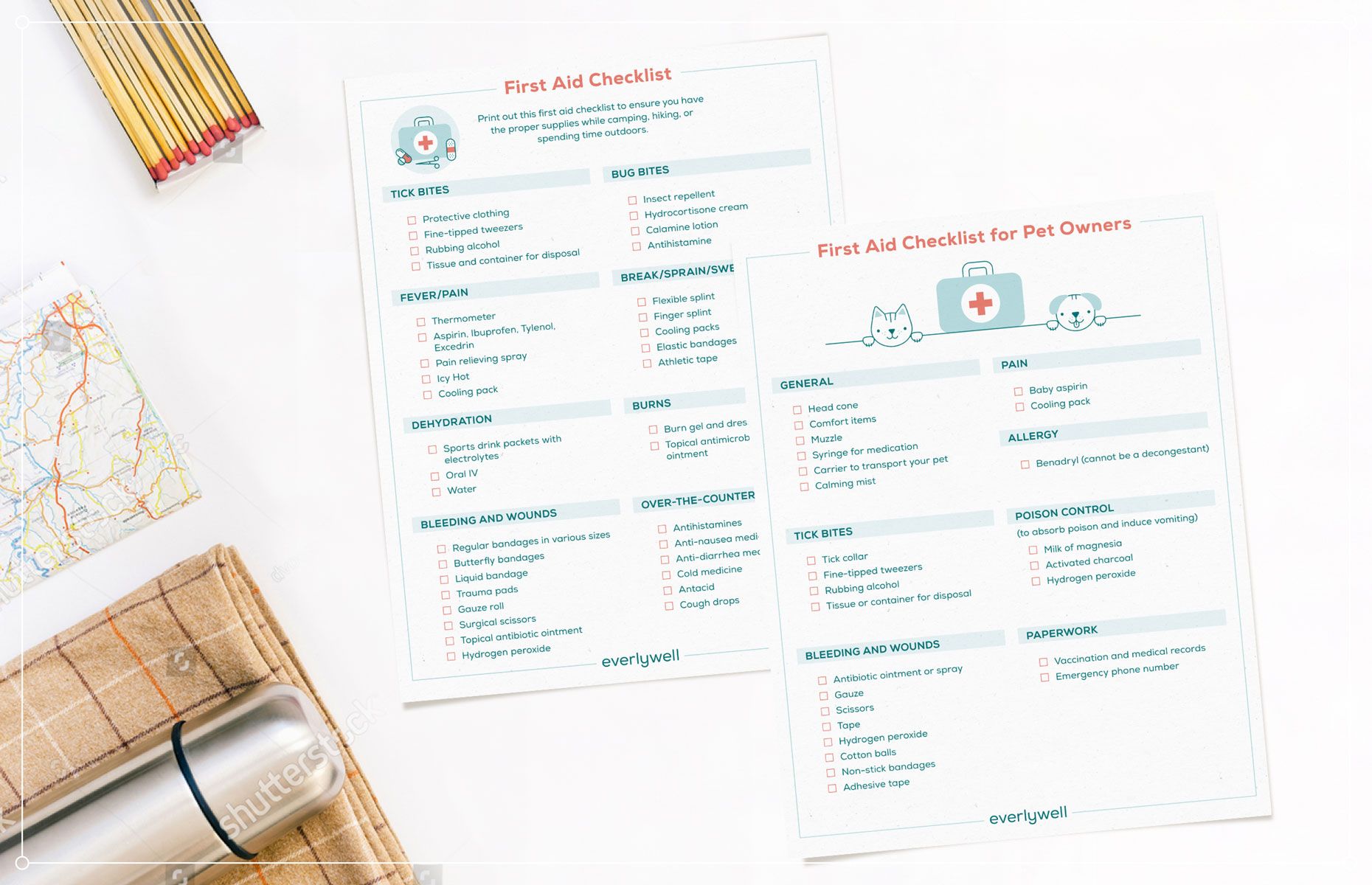
Whether you’re at home or outdoors, it's important to be prepared for any emergency. This starts with having the proper tools and equipment to handle anything from minor injuries to medical emergencies. You can print out and use the first-aid checklists (for humans and pets) below to ensure you’re prepared for the unexpected.
In the event that you are bitten by a tick, be sure you know how to safely remove it and when to see a healthcare provider if you are concerned about Lyme disease or Rocky Mountain spotted fever. If you’re at risk of contracting a tick-borne disease, we encourage you to visit your healthcare provider for an evaluation and/or treatment (and consider taking an at-home Lyme disease blood test.
Related content
What To Do If You're Bitten By A Tick
Types of ticks that carry Lyme disease
Article Sources
- Lyme Disease. Centers for Disease Control and Prevention. URL.
- Symptoms of Tickborne Illness. Centers for Disease Control and Prevention. URL.
- Lyme Disease Rashes and Look-alikes. Centers for Disease Control and Prevention. URL.
- Rocky Mountain Spotted Fever (RMSF). Centers for Disease Control and Prevention. URL.
- Lifecyle of Blacklegged Ticks. Centers for Disease Control and Prevention. URL.
- Lyme Disease Treatment. Lymedisease.org. URL.
- Lyme Disease. Mayo Clinic. URL.
- Signs and Symptoms of Untreated Lyme Disease. Centers for Disease Control and Prevention. URL.
- Lyme Carditis. Centers for Disease Control and Prevention. URL.
- Lyme Disease in Dogs: Tests, Treatment and Prevention. American Kennel Club. URL.
- Rocky Mountain Spotted Fever (RMSF): Transmission. Centers for Disease Control and Prevention. URL.
- Rocky Mountain Spotted Fever. Mayo Clinic. URL.
- Preventing Tick Bites. Centers for Disease Control and Prevention. URL.
- Regulation of Skin: Applied Repellants. United States Environmental Protection Agency. URL.
- Find the Repellant That Is Right For You. United States Environmental Protection Agency. URL.
- Using Insect Repellants Safely and Effectively. United States Environmental Protection Agency. URL.
- Surveillance, Spectrum, and Burden of Tick-Borne Disease, and At-Risk Populations. National Library of Medicine. URL.
- Preventing Ticks on Your Pets. Centers for Disease Control and Prevention. URL.
- Preventing Tick Bites. Centers for Disease Control and Prevention. URL.