
Medically reviewed on November 22, 2022 by Jordan Stachel, M.S., RDN, CPT. To give you technically accurate, evidence-based information, content published on the Everlywell blog is reviewed by credentialed professionals with expertise in medical and bioscience fields.
Table of contents
- Chlamydia basics
- 8 methods for preventing chlamydia
- How is chlamydia treated?
- Is there a vaccine for chlamydia?
- Keep tabs on your sexual health with Everlywell
- Related content
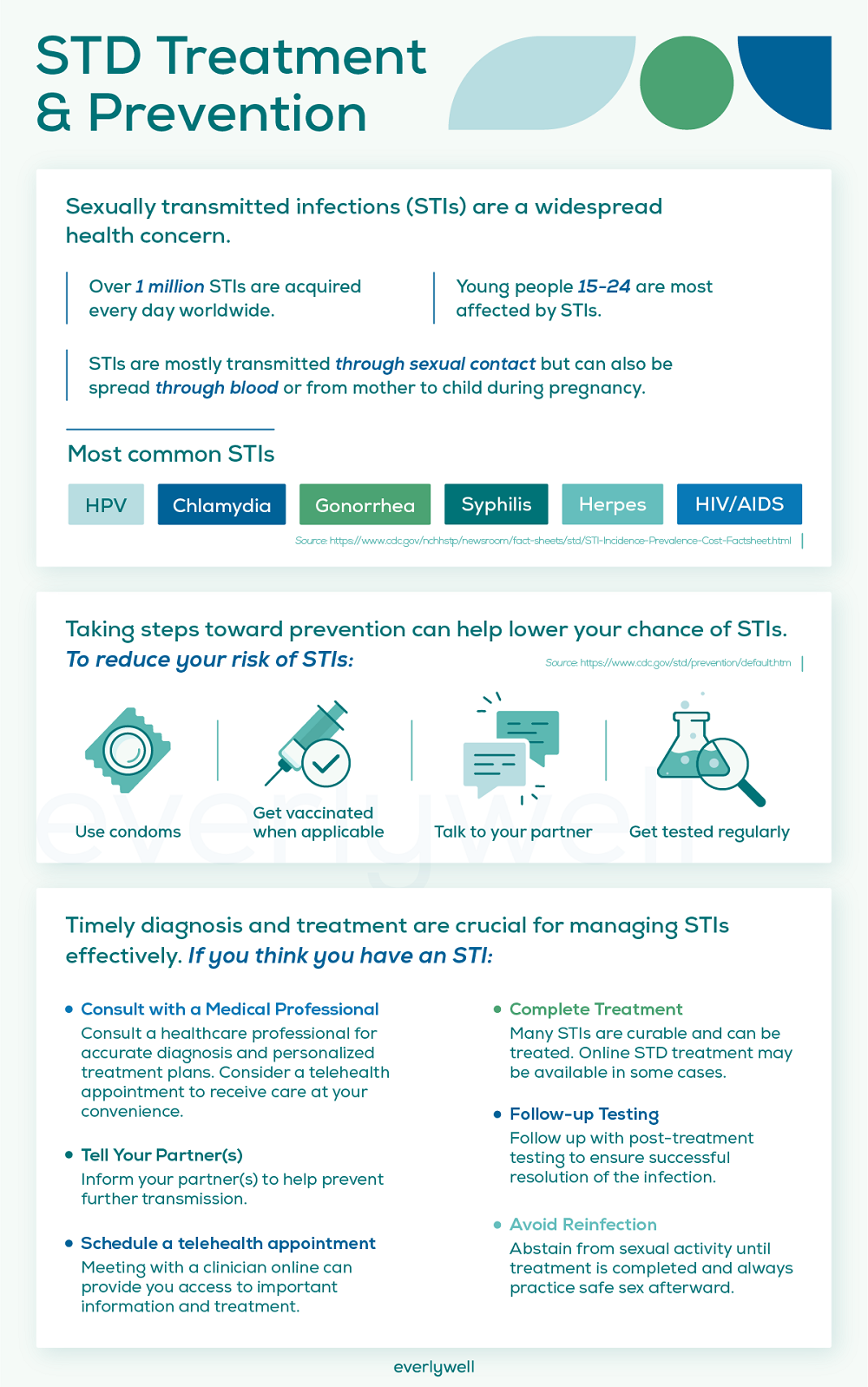
The first time chlamydia crossed your radar may have been high school sex ed.—just one of many STIs your teacher cautioned you and your classmates against. And while practicing safe sex is crucial for preventing any infection, it’s not always easy to distinguish between every sexually transmitted infection (STI) in the world of sexual health.
Chlamydia, however, deserves our special attention. As the single most reported sexually transmitted infection (STI) in the US, cases have risen so steeply in recent years that the CDC declared it an epidemic in 2015 [1]. For this reason, many people are now concerned with how to prevent chlamydia.
That said, there is some good news about this STI: chlamydia is treatable once properly diagnosed. And perhaps the best way to manage it is to know precisely what it is and which safe sex practices can help reduce your risk of contraction.
Chlamydia basics
Chlamydia is caused by a bacteria known as Chlamydia trachomatis, which is estimated to infect some 131 million people annually [2,3,4]. Though chlamydia can be contracted by people of any age, it predominantly occurs in young people between the ages of 15 and 24 [5].
One of the main reasons why the chlamydia trachomatis infection is so prevalent is because it’s often passed between partners who exhibit no symptoms of the infection. However, it can still have some adverse health consequences even if you are asymptomatic.
Is chlamydia dangerous?
The threat chlamydia poses to human health depends entirely on how far it progresses. Depending on who contracts it, chlamydia may result in several adverse health consequences when untreated [3]:
- In people assigned male at birth – Two health consequences are relatively common for men who contract chlamydia: prostatitis and epididymitis. Prostatitis is an infection of the prostate gland, while epididymitis is an inflammation of the testicles.
- In people assigned female at birth – When women contract chlamydia, they’re at risk of several adverse health effects ranging from infertility (caused by fallopian tube scarring) to pelvic inflammatory disease (PID). Additionally, women with chlamydia are at higher risk of ectopic pregnancy.
Pregnant individuals risk adverse health effects to themselves and their unborn or newborn baby. Chlamydia can be passed on to newborns, leading to lung infection (pneumonia) or serious eye infection [3].
8 methods for preventing chlamydia
Like many STIs, the only surefire way to fend off chlamydia is to abstain from sex—but we all know that’s unrealistic for many. (Besides, maintaining a healthy sex life has been associated with a stronger immune system, higher-quality sleep, and a sunnier mood) [6].
Fortunately, these 8 methods can help prevent chlamydia through safe sexual practices.
Use a condom
Unprotected sex can increase your risk of contracting chlamydia, or other STIs. That’s why one of the most effective ways to avert chlamydia is by using a barrier method of birth control—specifically, a male condom. Even though condoms aren’t foolproof, if used appropriately, they can curb your chances of contracting chlamydia by 75% [7,8].
Moreover, there are several ways to enhance condoms’ efficacy in preventing chlamydia:
- Store them properly – Carrying a condom in your wallet or your back pocket may work for a short period, but it can lead to rips and tears that could escape your notice. In general, try to keep your condoms in a dry, cool place (not in tight nooks) [7].
- Choose the best material – The most effective material for condoms is polyurethane or latex condoms [9].
- Check the expiration date – Before using one, check the packaging of your condoms to ensure they haven’t expired. If they’re on the older side, it may be worth inspecting them to confirm they don’t contain any defects [9].
- Use a lubricant – Using a sexual lubricant can lighten up friction, which may help to reduce the risk of condom breakage and failure [7].
Use a dental dam
Because chlamydia can be transmitted through oral sex, you may want to use a dental dam if you’re unsure of your partner’s status. Dental dams use a thin piece of material, usually latex, to protect against chlamydia by keeping bodily fluids from mixing [10].
In addition to chlamydia, dental dams can also help prevent [10]:
- Gonorrhea
- Syphilis
- HIV
- Hepatitis
Just remember that dental dams do not offer protection against HPV and genital herpes [10].
Avoid douching
For many people assigned female at birth, douching might seem like it could offer a measure of protection against chlamydia and other STIs.
However, according to The Office on Women’s Health, washing your genitals with a combination of water and purportedly “cleansing” fluids may increase your risk for STIs like chlamydia [11]. This is because your vagina contains many healthy strains of bacteria that can help keep the risky ones at bay (including Chlamydia trachomatis).
To that end, it’s best to skip douching altogether and allow your vagina to maintain its natural microbiome.
Skip the spermicide
One of the biggest myths about preventing chlamydia is that water-based spermicides can help shield you from it. In reality, studies indicate that one of the primary active constituents in commercial spermicides, nonoxynol-9, is ineffective at preventing the transmission of chlamydia [12].
So, if you use spermicide, bear in mind that it may not keep you from contracting this STI.
Clean your toys
If sex toys are a part of your sex life, remember that these are capable of transferring Chlamydia trachomatis between you and a partner [13].
With that in mind, be sure to incorporate the following hygiene practices to protect yours from harmful bacteria:
- Wash and disinfect your sex toys after each use
- Avoid sharing your sex toys with people you aren’t intimate with
- Consider applying a condom and lubricant to penetrative sex toys
- If you have multiple sexual partners, be sure to use the same toys with certain individuals (no sharing)
Know what symptoms to look for
As mentioned, chlamydia often goes undetected because some of its symptoms may go unnoticed. Knowing which signs of chlamydia to keep an eye out for can help you spot the disease before it advances.
If you were assigned female at birth, some common symptoms of chlamydia include [3]:
- Pain during sex
- Bleeding after sex
- Pelvic pain
- Vaginal bleeding between menstrual cycles
- Vaginal discharge
If you were assigned male at birth, the following symptoms could indicate chlamydia infection [3]:
- Penile discharge
- Pain in the testicles
- A burning sensation when urinating
If you notice any of these symptoms, it’s time to get tested. The sooner you can detect and treat a chlamydia infection, the lower chances of severe health consequences for you and your partner(s).
Get STI screenings regularly
Getting tested for STIs regularly is foundational for preventing any STI—especially if you’re sexually active and if you have more than one sexual partner. To protect against chlamydia, the CDC recommends being tested at least once a year (particularly if you have multiple partners) [14]. It's easy to take an at-home chlamydia test through Everlywell.
Furthermore, if you have a history of other STIs, you may have an elevated risk of contracting chlamydia [3]. At your test appointment, it’s recommended you also undergo screening for gonorrhea and syphilis [3].
Talk with your sexual partners
Candid conversations about your sex life are one of the keys to ensuring you’re safe and healthy. Make it a point to talk with your sexual partner(s) about:
- Their history of STIs
- Their history of partners with STIs
- Whether they currently have other sexual partners
- How often they get tested for STIs
- Their history of drug use
How is chlamydia treated?
Practicing these sexual health guidelines can help to lower your and your partner(s)’ risk of chlamydia, but there are occasions when infection can still occur. Fortunately, if you test positive for chlamydia, the infection is usually treatable with antibiotics.
If you're unsure how to treat chlamydia, the CDC suggests: [15]:
- Immediately telling your partner(s) about your diagnosis
- Using medications exactly as prescribed
- Not sharing medications with your partner or another person
- Abstaining from sexual activity for at least 7 days, even if you’re prescribed a single-dose antibiotic treatment
How long does chlamydia last? Following your antibiotic protocol, it’s recommended you take another test three months after your treatment—even if your partner(s) have been screened, treated, and cleared. This is important because roughly 2/3 of people can carry chlamydia without knowing it, and rates of re-infection are frequent [16].
Is there a vaccine for chlamydia?
As of 2022, we’re still waiting for a chlamydia vaccine. A potential chlamydia vaccine made headlines in 2019, when the first round of vaccine trials successfully triggered a human immune response against chlamydia trachomatis [4].
In the coming years, experts hope to have clearance to vaccinate children between the ages of 11 and 12 years old against chlamydia (the same way we vaccinate against HPV). But since it’s not yet clear when the trial vaccine will be released, using the tactics we’ve outlined above are the best tools we have in our sexual health toolkit for keeping ourselves and each other chlamydia-free.
Keep tabs on your sexual health with Everlywell
If today’s statistics on chlamydia teach us anything, it’s that testing is one of our most effective tools for preventing the spread of STIs. But busy schedules, long wait times, and slow turnarounds can make it challenging to keep up with screenings.
Everlywell Sexual Health Tests eliminate the practical challenges that keep us from prioritizing our sexual health. At-home test kits like the Chlamydia & Gonorrhea Test (or comprehensive STD Tests for Females and Males) let you learn your status from the comfort of home.
Related content
Untreated chlamydia in men and women
References
- CDC – chlamydia statistics. Centers for Disease Control and Prevention. Published April 12, 2022. URL
- CDC – Chlamydia – CDC Detailed Fact Sheet. Centers for Disease Control and Prevention. Published June 6, 2022. URL
- Chlamydia trachomatis. Mayo Clinic. Published February 11, 2022. URL
- Abraham S, Juel HB, Bang P, et al. Safety and immunogenicity of the chlamydia vaccine candidate CTH522 adjuvanted with CAF01 liposomes or aluminium hydroxide: a first-in-human, randomised, double-blind, placebo-controlled, phase 1 trial. Lancet Infect Dis. 2019;19(10):1091-1100. doi:10.1016/S1473-3099(19)30279-8
- STI prevalence, incidence, and cost estimates. Centers for Disease Control and Prevention. Published February 18, 2021. Accessed November 3, 2022. URL
- The Benefits of a Healthy Sex Life. Center for Women's Health. Accessed November 3, 2022. URL
- How often do condoms break? Planned Parenthood. Accessed November 3, 2022. URL
- Condom Fact Sheet. USAID. Accessed November 3, 2022. URL
- How to use a male (external) condom. Centers for Disease Control and Prevention. Published February 10, 2022. Accessed November 3, 2022. URL
- What is a Dental Dam & How to use it. Cleveland Clinic. Accessed November 3, 2022. URL
- Douching. Office on Women's Health. Accessed November 3, 2022. URL
- Kappus EW, Quinn TC. The spermicide nonoxynol-9 does not inhibit Chlamydia trachomatis in vitro. Sex Transm Dis. 1986;13(3):134-137. doi:10.1097/00007435-198607000-00004
- Chlamydia: Causes, symptoms, treatment & prevention. Cleveland Clinic. Accessed November 3, 2022. URL
- Which STD tests should I get? Centers for Disease Control and Prevention. Published December 14, 2021. Accessed November 3, 2022. URL
- CDC – Chlamydia treatment. Centers for Disease Control and Prevention. Published July 22, 2021. Accessed November 3, 2022. URL
- Crosby T. NIH grant funds Chlamydia Research. SIU News. Published September 7, 2018. Accessed November 3, 2022. URL
Spotlight on
Featured content

86% of cancers aren't caught by recommended screenings. See what they're missing with a single blood draw.
Save $100 now
Explore Everlywell









